With the COVID-19 pandemic placing unprecedented strain on health care systems around the world , so does it strike at the people in need of urgent medical care for other illnesses. Afraid that they may contract the virus outside of their homes, patients with chronic conditions like cancer, hold back on their symptoms and work-ups in order to avoid exposure in emergency rooms and even doctors’ clinics.
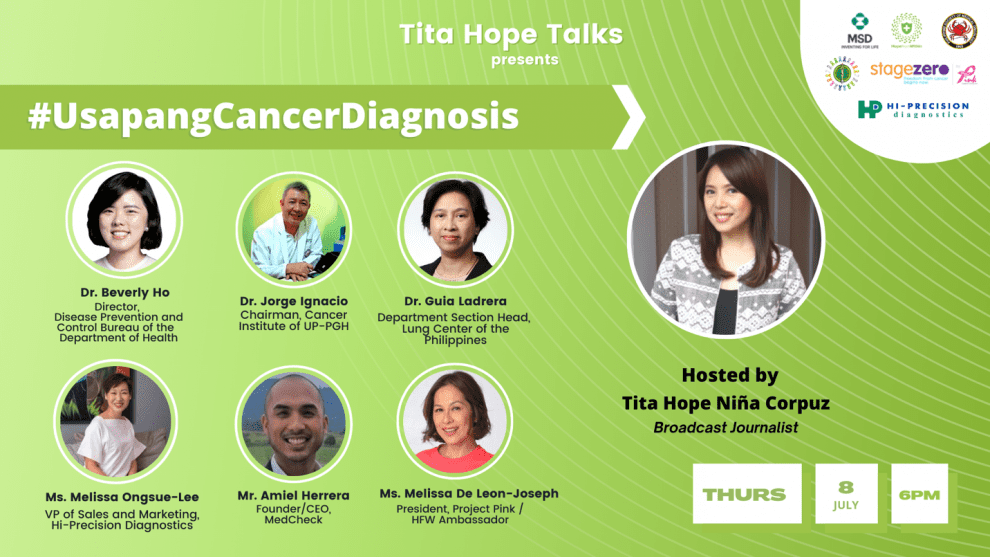
This concern is what Hope From Within, a multi-stakeholder cancer advocacy campaign spearheaded by MSD in the Philippines, sought to address in its second episode of its cancer conversation series dubbed as ‘Tita Hope Talks’. Tackling Access to Cancer Diagnosis and Navigation in the COVID-19 Era, the discussion highlights the importance of early diagnosis in cancer care, with or without pandemic. Through this episode, Hope From Within seeks to remind the public to consult their doctor as soon as they spot something unusual and not to put off preliminary screening. Afterall, spotting cancer early increases the chances of survival.
Hosted by broadcast journalist and health advocate Niña Corpuz, ‘Tita Hope Talks’ gathers experts and health stakeholders to discuss their perspective and provides their insights on various issues surrounding cancer care. This session’s panel of speakers include Dr. Beverly Ho, Disease Prevention and Control Bureau Director of the Department of Health; Dr. Jorge Ignacio, Cancer Institute Director of the UP-PGH; Dr. Guia Ladrera, Oncology Department Section Head of the Lung Center of the Philippines; Melissa Ongsue-Lee , VP for Sales and Marketing of Hi-Precision Diagnostics; Amiel Herrera, Founder/CEO of Medcheck; and Melissa De Leon, President of breast cancer support group Project Pink.
The (added) challenge of battling cancer today
The role of cancer screening in early detection and its impact on survival is well documented in breast, cervical, lung, and colorectal cancers.
However, for the first time, cancer screening has been globally interrupted. As the number of new COVID-19 cases and related deaths increases, interruptions of cancer screening schedules became inevitable.
This presents oncologists with some unprecedented challenges. It is anticipated that the gap in cancer screening will result in delayed diagnoses, an increased proportion of patients presenting with advanced disease, delays in treatment, and eventually, detrimental effects on survival.
For instance, the PGH Cancer Institute shared that pre-pandemic, the hospital would cater to an average of 120 patients daily. But in 2020 onwards, an average of 20% of cancer patients have not returned for their regular treatments, and some have already relapsed. Some facilities in other hospitals even had to close down as medical attention was channeled toward COVID-19.
Screening: A preventive measure for cancer
According to WHO, cancer detected at an early stage gives the best chance of survival. But when management is delayed, patients are more likely to meet greater problems and higher costs of care.
One way to be more conscious of one’s health condition is to do regular screening. Compared to early diagnosis, screening is a totally different strategy that checks on illnesses that might be present, even if one is presumed healthy.
There are three Rs that need to be assessed when doing cancer screenings — risk factors, recommendations, and rationale. By constantly being in check of one’s health, the effects of cancer on personal and economical aspects can be reduced.
Unfortunately, many patients overlook the cancer screening process due to multiple factors. Some are worried that they might test positive for cancer, others fear the procedure itself, some are unaware of where to go and how to book a screening schedule, and to a huge chunk of patients, they view screenings and check-ups as another financial burden for their families.
Leading types of cancer and available screening programs
Breast cancer remains to be the leading cause of cancer-related deaths among women. Currently, the Department of Health offers the Breast Cancer Medicines Access Program (BCMAP) in government hospitals to support indigent cancer patients. The BCMAP aims to promote early breast cancer screening particularly among poor women by providing assured access to medicines as well as psychosocial support.
The free medicines access program for cancer is not only meant to provide ready access to cancer medicines but to promote early-screening and cancer awareness among Filipinos emphasizing that detecting, treating and managing cancer in the early stages improves the overall prognosis and survival rates for patients.
Another leading cause of death among women is cervical cancer. It stands as the second most common cancer type in Filipino women next to breast cancer. Several methods can be used for screenings such as the VIA (visual inspection using acetic acid) and pap smear. The DOH provides free cervical cancer screening provided every year in 58 DOH Hospitals done during the month of May to screen women ages 30-45 years of age.
Meanwhile, lung cancer is the second most common and the number one deadliest cancer among Filipino men and women. In 2020 alone, 19,180 Filipinos have been diagnosed with lung cancer; of these, 17 063 resulted in death. Surprisingly, despite these alarming statistics, there are no screening programs existing for lung cancer.
A glimmer of hope of cancer patients
While the costs of health care in the country remains to be a top concern for a great number of Filipinos, MSD’s ‘Tita Hope Talks’ sheds light on the continuous progress in providing Filipino patients better access to cancer care. The signing of the Republic Act No. 11215, otherwise known as the National Integrated Cancer Control Act (NICCA), aims to augment cancer survivorship by strengthening essential programs throughout the whole cancer care scope.
The Cancer Law the establishment of the Philippine Cancer Center for patients to have a ground-zero for top-quality cancer treatments. And to help Filipinos with finances, a Cancer Assistance Fund is also in the works to complement the implementation of the Universal Health Care Act. It also expands PhilHealth packages for Filipinos diagnosed with cancer.
If implemented right and funded properly, the NICCA will give better support to cancer patients, especially those from the underserved throughout every step of their cancer patient journey – from diagnosis, to getting access to treatment options, and to getting post-cancer care all while ensuring that the entire journey isn’t as physically, emotionally, and financially burdensome as it is typically known to be.
To know more about MSD’s Tita Hope Talks discussion on Access to Diagnosis, watch the second episode via Hope From Within’s Facebook Page at https://www.facebook.com/Hopefromwithinph or through their official website https://hopefromwithin.org/.